Childhood Cancer and Inequalities – why we invest in pediatric care
Cancer remains the leading cause of disease-related death for children and nearly half a million of them around the world received the much-dreaded diagnosis last year – mostly leukaemia, brain cancers, lymphomas and solid tumours.
On International Childhood Cancer Day – the global campaign to raise awareness of paediatric cancer – we reflect on the road ahead: from the phenomenal advances in research, to the alarming disparities in care access.

Acute lymphoblastic leukaemia (ALL) was uniformly lethal in children prior to the 1950s. Today, more than 90% of them are cured. The progress in the last decades has been prodigious. CAR-T cell therapies are demonstrating their versatility, particularly in children with very advanced forms of leukaemia and cancers with lower mutation loads. We have had tissue agnostic drugs enter the market, such as NTRK inhibitors, for children with solid tumours that harbour a specific genetic alteration. However, some cancer types have seen limited improvements in treatments and outcomes. This is where mRNA strategies, that came to fame in the last two years, offer the promise of personalised vaccines for cancers that carry high numbers of mutations, such as lung and bowel cancer, which are still often fatal.
Developing strategies for paediatric cancers that either have no effective treatments, or have treatments but with unacceptable toxicities, involves unique challenges. While some cancers are seen in children and adults, other cancers are essentially only seen in children, and the four most common adult cancers (lung, breast, prostate, and colorectal) are largely absent in children. Hence, improving outcomes for children begins by recognising the many fundamental differences between childhood and adult cancers, and the landscape in which new drugs are developed.
It calls for frontline doctors to be trained to pick up on the earliest symptoms and for international standards of care to include biomarker screening in children. Misdiagnosis or late diagnosis are by far the leading causes of treatment failure for children with cancer. By prevalence, paediatric cancer is a rare disease and 94% of physicians feel ill-equipped to detect it, which leads to half of patients remaining undiagnosed for years. As with adults, the earlier the detection, the higher the chance of recovery.
Powerful diagnostic platforms are now being made available to clinicians worldwide to allow the right treatment to get to the right patient in a timely manner. Some companies offer whole-genome analysis to detect genetic disease predisposition in children (e.g. Congenica in Cambridge, UK). Others uncover disease signatures based on imaging biomarkers capable of detecting and staging the most lethal paediatric tumours without the need to put kids through invasive tissue biopsies (e.g. Quibim in Valencia, Spain). These technologies can precisely locate the cancer in the body and monitor the efficacy of treatment options. They also generate important information on the interactions between onco-cells and the cells in their surrounding environment. By bringing molecular and cell biology information together one can look at tumours as an ecosystem — critical for developing combinations of drugs that might be able to keep cancers at bay and transform them into more manageable chronic diseases.
Clinical decisions will be made on a case-by-case basis. There may be new therapies, we mentioned a few promising ones earlier, but researchers can also opt to combine existing drugs. Scientists at Healx (Cambridge, UK) can analyse millions of drug and disease data points to find novel connections and turn them into treatment opportunities. But this heterogeneity in therapeutic options creates new logistical challenges. For instance, with cell and gene therapies each patient requires not just their own treatment, but also a unique delivery process. Teams like OriBiotech (London, UK) have developed technology platforms that automate and standardise manufacturing at the hospital, allowing therapeutics developers to bring their products directly to the patient. This revolution in accessibility of new treatment modalities is wonderful news for children and their families.
Despite this progress, any discussion of advancement also requires that we recognise where disparities remain. For some paediatric cancers, such as those affecting soft tissue and the central nervous system, long-term survival is still poor and treatment advances have been limited. Also, children cured may face a lifetime of health problems caused by their disease and its treatment (aggressive surgeries, radiation, and chemotherapy), including hearing loss and infertility.
Let us take this opportunity to remember that in health too we are far from equal. Socio-economic stratification and cultural biases have drastic consequences on a child’s chance of survival. The World Health Organization reminds us that inequalities in health and social injustice are killing people on a grand scale.
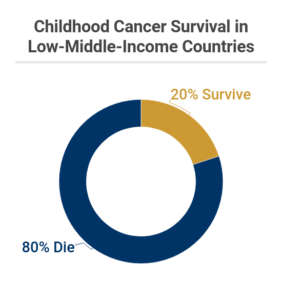
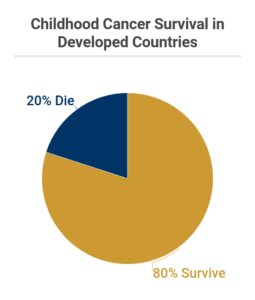
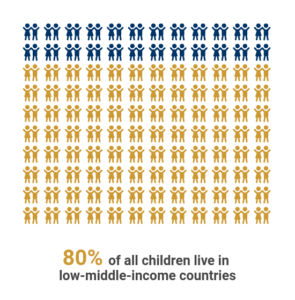
While 80% of children survive cancer today in rich countries, merely 20% are lucky enough to make it through in low to middle income geographies. This is appalling because the treatments exist, and what’s more alarming is 80% of the world’s children live in these countries.
The picture isn’t flattering either in developed countries where the gender and ethnic divides run deep. A study following 67,000 American children with cancer found that those from racial and ethnic minority groups are less likely to survive cancer than their white counterparts: Hispanic kids with the same tumour types were 63% more likely to die, and black children 59%. Gender discrimination in treatment is another challenge: researchers working on Irish national data covering 3,700 children observed that girls were significantly less likely than boys to receive radiotherapy for leukaemia overall and acute lymphoblastic leukaemia specifically, as well as surgery for central nervous system (CNS) cancers.
It’s a stark reminder that there is only so much science can do. Researchers move mountains, only for patients to be prevented from accessing life-saving treatments because of societal norms, ethnicity, religious views and, of course, wealth inequality.
Much remains to be done for the right treatment to reach the right child.
